ICATA Journal
Cognitive Analytic Therapy in the provision of care for mental health staff in an Employee Psychology Service
Sarah Craven-Staines
Cite as: Craven-Staines, S. (2019). Cognitive Analytic Therapy in the provision of care for mental health staff in an Employee Psychology Service. International Journal of Cognitive Analytic Therapy and Relational Mental Health, 3(1), 94-105. https://www.internationalcat.org/volume-3-6
Int. Journal of CAT & RMH Vol. 3, 2019 / ISSN2059-9919
Abstract
The recognition of burnout amongst staff working within mental health services is not a new concept. Yet the ability to support the mental wellbeing of our staff has been limited and variable in nature dependent upon the service in which they work. In 2015, a large mental health trust in the North East of England recognised the mental health needs of staff given the growing numbers of sickness absence relating to work-related stress, anxiety and depression. In response, the Trust agreed to pilot an Employee Psychology Service, to provide staff access to clinical psychologists and psychological therapies, with an aim of supporting staff experiencing work-related stress. The following article is a reflection upon how Cognitive Analytic Therapy (CAT) can be used in such a service, to offer therapy individually to staff members as well as with staff teams within the wider organisation. This article reports significant differences in pre and post outcome measures from a small sample size (n=15) of staff clients; as well as qualitative quotes recognising the value of using CAT in organisations.
Keywords: Cognitive Analytic Therapy; Staff; employee support; mental health; team reformulation
Introducing work-related stress
Cartwright and Cooper (1997) identified that there are six general categories, which can be triggers of work-related stress. These are: factors intrinsic to the job itself (physical environment, workload, working hours etc.); roles in the organisation (e.g. role responsibilities, role ambiguity, conflict, overload); social relationships at work (e.g. with supervisors, colleagues, clients etc.); career development; and organisational development. Similar stressors are seen as the precipitating factors that, lead staff to being referred to the EPS. Whilst it is recognised that the aim is to focus upon ‘work-related stress’, often this does not come without ongoing or existing difficulties within the staff member’s life outside of work, or in their own historical background.
The persistence of work-related stress can often lead on to burnout and depression in staff. Maslach (1982) reported that ‘burnout’ is the experience of emotional overload and exhaustion, which occurs when people become closely involved and feel over-burdened by the emotional demands of working with people who are distressed. Often individuals reach a point of feeling ‘drained’ and as a result lack the energy or motivation to continue to work. Maslach (1982) highlighted that if such a situation continues to occur, there is a risk that the staff member will become detached from emotional involvement with the clients they are working with, as a means of coping. Walsh and Walsh (2009) reviewed the existing literature to investigate the risks mental health staff face to their own mental health and found that contributing factors included frequent contact with severely ill patients, organisational change, uncertainty about role and low support.
CAT as a framework to conceptualise work-related stress
Walsh (1996) used CAT to consider the roles that staff members can often be caught within in relation to themselves and others when working within the helping professions. She acknowledged that when things go well, staff can often feel worthy and valued. However, should situations become difficult, individuals could be left to feel minimised, useless or worthless. Staff are often drawn into a helping professions role through the desire to care and for others to feel gratefully cared for (Lloyd, 2011).
As the political climate of the NHS continues to change, staff face increasing demands, tight deadlines, and mounting targets. Jones and Childs (2007) discussed the reforms in the NHS through a CAT lens, in writing a reformulation letter. In doing so, they identified numerous reciprocal roles that staff face, such as controlling–controlled, threatening – powerless and dismissing–ignored. Such roles often leave staff feeling overlooked and without a voice to express how they are feeling. Prioritising staff ’s own need for care, therefore, becomes a necessity in an environment where individuals are struggling to cope and maintain their workload, resulting in increased rates of sickness. Managers within the Trust that this article refers to, are aware of such need to reduce sickness absence, and therefore are often willing to invest in time spent to support staff and their mental wellbeing.
Whilst staff often view managers as those in the ‘pain inducing’ end of the reciprocal roles (e.g. controlling, threatening, dismissing), CAT can be helpful in supporting both staff and managers to understand the interacting systems that they can all be drawn into. A shared under- standing can acknowledge unhelpful dynamics due to the external pressure placed upon all staff within their differing positions. As a result, acknowledgement of how managers also encounter the ‘pain experiencing’ end of the role can be helpful to allow staff to recognise the reciprocity in roles. Carson and Bristow (2015) spoke of the importance of collaborating with NHS management to aid change.
My own position within the Employee Psychology Service
After having worked for 9 years post qualification in a Community Mental Health Team for Older People, I took a change of career some two years ago and began a split post as Academic Tutor for the Doctorate in Clinical Psychology Programme at Teesside University as well as working as a Clinical Psychologist within the Employee Psychology Service. As a CAT practitioner, and with a strong belief in the applicability of CAT to different settings, I felt that there would be a lot for CAT to offer through being utilised within the EPS. My role not only entailed meeting staff on a 1:1 basis for direct therapy, but also working with teams in distress, who were struggling to function and had high sickness rates.
Conclusion
Delivering a service that supports our employees in their mental health and wellbeing is a new venture and one that is proving worthwhile. Psychology has a lot to offer our employees as they face a huge amount of pressure from the organisational systems around them, whilst also facing their own personal challenges in life. The use of CAT within the EPS is only one area in a wider whole, with other staff members practising different therapeutic approaches. CAT, however, has a valuable position in working with staff both individually and within wider groups, as it offers a non-judgemental, collaborative and reciprocal way of working that can help normalise and understand the tensions staff face in their daily practice. It is hoped that this reflective piece is one of more to come, as the service develops and the outcome data grows in using CAT with staff groups. The use of CAT within the organisation is continuing to be promoted and staff will be encouraged to reflect upon the value of working with an observing eye on relational processes.
The use of CAT directly in 1:1 therapy with staff
I was aware that the pace of working with staff clients would be different to working with older adults. Not only has there been a high demand for EPS, with increasing referrals each month, there was also recognition that the period of work should be shorter in nature. For the first time in my career, I was beginning to become familiar with working within contracts of 8 or 12 session CAT, much shorter than I had previously been used to. Despite this, what I did find was that given that I was now working with staff, they had a wealth of psychological knowledge, as the majority were clinical staff and embedded within multidisciplinary teams of their own. Whilst many had not worked directly using CAT, they understood concepts relatively easily, which helped with the shorter time frame.
Staff often came to the EPS with an ongoing work-related difficulty (often increased demands upon role, working over and above contracted hours to meet such demands, difficulties in relationships with teams and managers, or change to structure of teams). However, generally through deeper discussion, staff clients often reported difficulties within their personal lives (e.g. relational problems or breakdown, past abuse and increased strain on home life). Often the work-related stress, personal difficulties and past life events sat hand in hand, as the problematic patterns they were becoming caught within, naturally mirrored one another. This is a similar reflection to that which Appleby (2003) made in working within an occupational health department. She too recognised that whilst the main precipitant for staff may be a work-related problem, a personal issue is also often present, and there can frequently be links made with much earlier pain.
For staff clients seen within EPS, there were often competing pressures with a desire to ‘perfectly care for’ others versus frequently feeling ‘criticised’, ‘crushed’, ‘overwhelmed’, ‘shamed’ and ‘powerless’. Such feelings were experienced in relation to the organisation and manage- ment, as well as the self when increased demands are unable to be sustained. The pain-experiencing end of reciprocal roles highlighted within the sequential diagrammatic reformulations (SDRs) throughout therapy, naturally linked to past experiences, and often as a result, the work-related stressor was a trigger for the core pain.
The benefit of CAT in this instance is its reciprocity and ability to collaboratively draw together an understanding of core pain, its foundation and how it continues to re-emerge in day-to-day situations. Staff clients often reported that creating an understanding of their reciprocal roles and problematic patterns was vital for the change process to begin to occur. Commonly, the stage of recognition before revision, led staff to feel uncertain and anxious about how to make change, yet their motivation outside of sessions to begin to recognise and seek revision often led to movement and modification occurring relatively quickly.
In the 2 years of working 1 day per week in the service, 20 staff completed CAT interventions. Pre and post objective measures were used to assess staff wellbeing post therapy and full data is held for 15 staff. Measures used were: Generalised Anxiety Disorder – 7 (GAD-7; Spitzer, Kroenke, Williams, et al., 2006); Patient Health Questionnaire – 9 (PHQ- 9; Kroenke, Spitzer and Williams, 2001) and the Work and Social Adjustment Scale (WSAS; Mundt, Marks, Shear and Griest, 2002). It is often seen in EPS that staff under-report distress in initial sessions for fear of being seen as incompetent or unable to fulfil their roles. This, therefore, needs to be taken into consideration when analysing the data. Whilst the numbers of pre and post outcome measures are limited, paired sample T-tests were conducted to identify any significant differences between pre and post therapy aggregate scores (for the GAD-7; PHQ-9; WSAS).
There was a significant difference in scores for the GAD-7 pre therapy (M=11.18; SD=5.54) and GAD-7 post therapy (M=3.06; SD=2.71) scores; t=(14)5.5, p<0.01. Similarly, significant differences in scores for the PHQ-9 pre therapy (M=13.18; SD=8.68) and PHQ-9 post therapy (M=3.31; SD=2.75); t=(14)4.3, p<0.01 were found. Finally, there was a significant difference in scores noted for the WSAS pre therapy (M= 19.12; SD=12.31) and the WSAS post therapy scores (M=4.18; SD=3.41); t=(14)4.7, p<0.01.
Table 1: Breakdown of significant pre and post measures using T-tests

The preliminary findings are encouraging and indicate a significant reduction in scores on each objective measure post therapy in comparison to pre therapy. Individuals’ scores on the GAD-7 showed a change from the ‘moderate’ range to the ‘mild’ range, whilst on the PHQ-9, scores reduced from the ‘moderate’ to ‘minimal’ range. Finally, for the WSAS, individuals’ scores reduced from the ‘significant functional impairment with less severe clinical symptomatology’ range to the ‘below subclinical population’. The preliminary findings are, however, open to limitations, particularly in terms of a lack of control group and thus the potential for naturally occurring positive change over time. Despite this, the findings were also backed up by positive qualitative feedback from staff:
‘I believe that with the tools you have given me and the talks we have had I am in a much better place to keep myself safe and on an even keel. I cannot express how highly I think of yourself, and the sessions we have had.’
‘The sessions have been invaluable. . . life changing in fact! Thank you so much for helping me to find ‘me’ again. Never to be forgotten!’
The contextual use of CAT within the EPS
The Employee Psychology Service also provides a broader, outward facing role, particularly in supporting wider staff groups who are struggling. Often, when teams have blanket targets and demands, or when difficulties arise in professional relationships, it is not one person alone who is struggling, rather the whole team. Therefore, offering CAT as an approach to reformulating problematic patterns within a system can benefit a wider approach to team functioning.
Appleby (2003) reflected upon how often there is similarity between pain, procedural coping strategies and reciprocal roles in clients, staff and managers. The understanding of projection of these onto one another and into the culture can often highlight how the whole system is behaving. She went onto describe that ‘problem’ areas in healthcare often occur when communication has broken down, and it is often seen that there isn’t time for staff meetings or training events. In doing so, teamwork and support begins to diminish, leading to splitting and a greater degree of helplessness amongst staff.
I worked for over 18 months with one of our corporate teams, who requested support at a point in which they were all beginning to experience a sense of burnout, and an inability to continue to function as they were. The team have provided consent for their experience and SDR to be shared within this article. Upon meeting them, staff had been working over and above their contracted hours, were taking work home to meet the specified targets, and were struggling to effectively use annual leave allocations (or coming into work on planned days off). The team felt at breaking point and were uncertain of how to move forward. It was recognised that a wider team approach was needed to understand the difficulties they were being drawn into. Management were also in support of this, prioritising the release of staff to attend meetings.
I offered a CAT reformulation meeting to map some of the difficulties they were facing and to begin to create a shared understanding of the obstacles they were encountering. Figure 1. provides the SDR developed in the first meeting. A number of different themes were identified that the team felt contributed to the position they had found themselves in. These included: the political climate of the NHS; changes they faced due to new national guidance documents; changes in managers and changes in their own job descriptions. Due to frequent transformation, they had at times felt unsupported and lacked direction by higher management. The increase in workload within the team had led to a mounting pressure to perform. Staff reflected upon the pride that they took within their roles, and thus how they often strived to make sure that all their work was to a high standard. Due to the increasing demand and pressures, however, they began to feel overwhelmed and would either become critical of themselves for feeling this way, or would withdraw and isolate themselves from the rest of the team, believing that they were alone in feeling like this and that others would be critical of them for not performing.
Patterns highlighted were similar to those of feeling overwhelmed and detached, as identified by Maslach (1982). Following months of work- ing over to meet targets, they reached a point of burnout. This reinforced a sense of internal criticism within staff members, as they would believe they were letting the team down. At times, the pressure the team felt from higher management was also met with criticism, as targets were re- enforced, and they felt singled out, if deadlines were not met.
Figure 1: Sequential Diagramatic Reformulation of team functioning
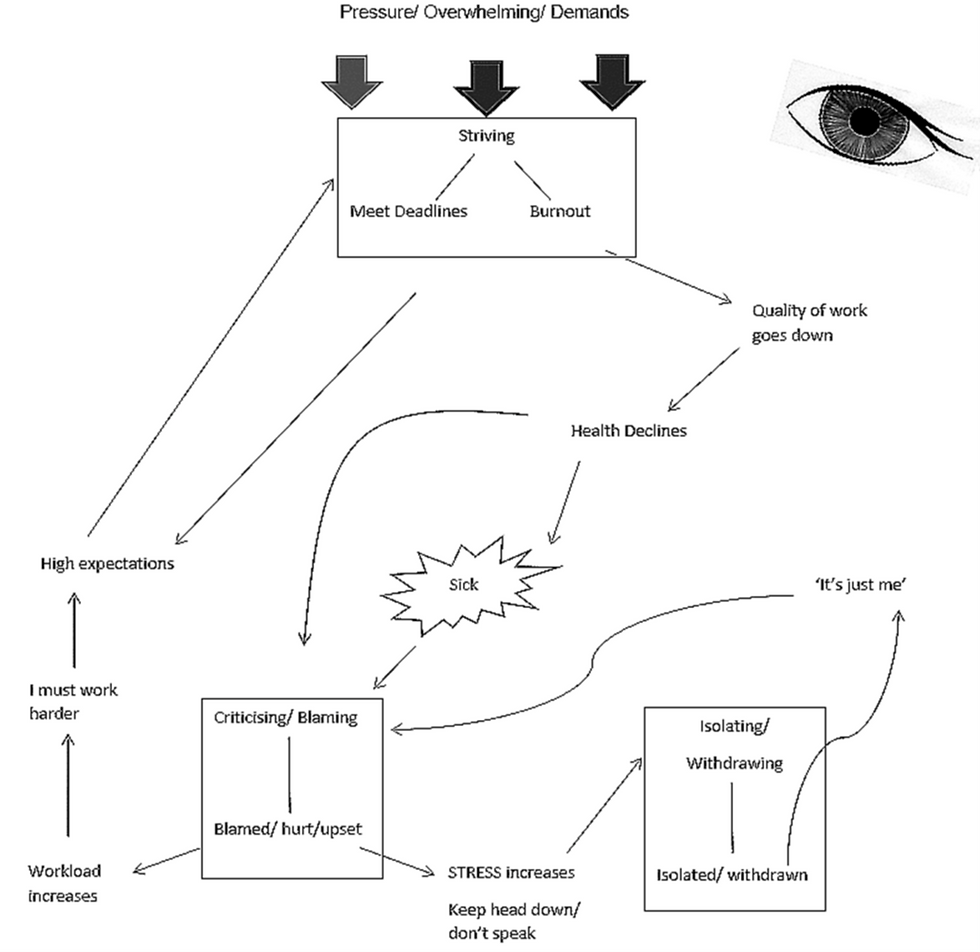
Staunton, Lloyd and Potter (2015) used the Helper’s Dance Checklist (Potter, 2013) to identify relational patterns within a learning disabilities service in a large Mental Health Trust. They found that staff often felt drawn into similar reciprocal roles to those identified here. Specifically, there was often a ‘striving to meet demands’ trap identified by staff coupled with reciprocal roles of criticising to criticised and judging to feeling judged, if such demands were unsustainable. There may therefore be universality to the problematic patterns and reciprocal roles experienc- ed by staff in the helping professions.
For this team, through opening a dialogue of the experiences they faced together and by beginning to map the maladaptive coping strategies that they had been drawn into, individuals began to reflect upon the value of bringing the unspoken into the open and how helpful it was to hear that they were not alone in feeling the way they did. The team were also keen to acknowledge their strengths. Despite their weakening morale, they noted the internal strength they felt as a team. They had an identity, a sense of closeness and a healthy banter that could reverberate around the office. The team felt secure and safe within the workplace and shared a hope that things could get better in the future.
We were keen to draw upon the strengths in the meeting and to acknowledge how the staff group could build on these. Identifying exits to the problematic patterns were also important and together the team agreed on: altering how they managed the referral process; being clearer on their workload and feeling able to say ‘no’ when demands became too much; getting feedback from one another on their work (to allow them to step out of striving to be perfect); if demand began to outweigh capacity having a direct link to the Executive Management Team through their own manager; and having space each week allocated as a team to de-brief on cases. We also acknowledged the importance of positively reinforcing the achievements they made, particularly through promoting them in the staff E-Bulletin and registering for team of the week.
The team have valued the input provided by psychology and the opportunity to consider some of their problematic patterns. They recognised that whilst some of their improvements had happened either before or in parallel with the CAT reformulation meeting, the SDR helped them recognise their problematic patterns and how to step out of them. They pinned their SDR on the office wall in order to keep an observing eye on the team and the patterns. The team reported that they could think of other teams who would benefit from the same experience. Some qualitative feedback received from the attendees suggested the value of having CAT reformulation meetings for teams:
‘I always felt invigorated after a CAT reformulation session as I felt listened to; it gave me the confidence to approach my line manager to discuss my workload without feeling guilty.’
‘The most important issues for me were to recognise when my “red flags” were starting to appear (working too many hours at home, not sleeping) and to be able to discuss these red flags within the group.’
The team agreed that routine meetings to reflect upon their SDR and exits would be beneficial and initially we arranged to meet every three months and then later on a six-monthly basis to review their progress. The team continued to face pressures and at times when we met, they recognised that they were back on the map and reflected upon whether or not they were still utilising the exits identified. In our more recent review, given the changing nature of the team with new staff members, the team requested to reformulate, mapping again any new procedures that they found challenging and seeking new revised exits from them. Overall, the CAT reformulation meetings provided staff with an opportunity to feel heard, valued, and supported. They were widely accepted and commended by staff. In addition, the CAT reformulation meetings allowed staff members to acknowledge pressures their own managers may be under and the reciprocity of the difficult roles.
References
Appleby, K. (2003). Cognitive Analytic Therapy - its influence on my practice in the Occupational Health Speciality within a Clinical Psychology and Counselling Service. Reformulation, Spring, 18-24.
Carson, R. & Bristow, J. (2015). Collaborating with Management in the NHS in difficult times. Reformulation, Summer, 30-36.
Cartwright, S. & Cooper, C. L. (1997). Managing Workplace Stress. Thousand Oaks, CA: Sage Publications. https://doi.org/10.4135/9781452233772
Jones, A. & Childs, D. (2007). Reformulating the NHS reforms. Reformulation. Summer, 7-10.
Kroenke, K., Spitzer, R. L., & Williams, J. B. (2001). The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 16(9), 606-13. https://doi.org/10.1046/j.1525-1497.2001.016009606.x
Lloyd, J. (2011). Consulting with staff teams. Clinical Psychology and People with Learning Disabilities. 9, 1. https://doi.org/10.53841/bpsfpid.2011.9.1.22
Maslach, C. (1982). Burnout: The cost of caring. New Jersey: Prentice Hall.
Mundt, J. C., Marks, I. M., Shear, K.& Griest, J. M. (2002). The Work and Social Adjustment Scale: a simple measure of impairment in functioning. The British Journal of Psychiatry. 180 (5) 461-464. https://doi.org/10.1192/bjp.180.5.461
Potter, S. (2013). The Helper's Dance List. In: Lloyd, J. and Clayton, P. Cognitive Analytic Therapy for People with Intellectual Disabilities and their Carers. London: Jessica Kingsley Publishers, 89-121.
Spitzer, R. L., Kroenke, K., Williams, J. B., et al. (2006). A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med. 166(10), 1092-1097. https://doi.org/10.1001/archinte.166.10.1092
Staunton, G. Lloyd, J. & Potter, S. (2015). Relational patterns amongst staff in an NHS Community Team. Reformulation, Summer, 38-44.
Walsh, B. & Walsh, S. (2009). Is mental health work psychologically hazardous for staff? A critical review of the literature. Journal of Mental Health. 10 (2), 121-129. https://doi.org/10.1080/09638230123742
Walsh, S. (1996). Adapting cognitive analytic therapy to make sense of psychologically harmful work environments. British Journal of Medical Psychology. 69, 3-20. https://doi.org/10.1111/j.2044-8341.1996.tb01846.x
Acknowledgements
Firstly, for making this paper possible, many thanks to the team I worked within, who have allowed their story to be shared in this article. I would also like to express my gratitude to Dr Kate Freshwater (Consultant Clinical Psychology), Dr Sarah Dexter-Smith (Director of Therapies) and Dr Ash Summers (Programme Director) for their support and guidance throughout the writing of this article. Finally, with great thanks to Dr Steven Muncer (Research Tutor) for his statistical knowledge and support.
Introduction to the Service
The Mental Health Trust, within which this work was completed, is committed to supporting the health and wellbeing of staff. As a result, after two years of pilot, a permanent service is available for staff who may be experiencing significant episodes of work-related stress, anxiety and/or depression. The Employee Psychology Service (EPS) has been running in the Trust since 2015 and is led by a full-time Consultant Clinical Psychologist, one Clinical Psychologist (author SCS) one day per week and a full-time psychological therapist (at the time of writing this article). Referrals are received from Employee Support Officers who provide support for staff experiencing difficulties in their health and wellbeing. Through an initial assessment within the EPS, a joint decision is made between the staff member and clinician about the therapeutic model used, based on client need and therapist availability.
The following article, aims to reflect upon the provision of Cognitive Analytic Therapy (CAT) within the EPS, recognising the uniqueness of CAT in providing both a relational and organisational approach to working with staff. Due to this, the article will form two main parts:
(a) reflecting on the use of CAT directly in 1:1 therapy with staff; and
(b) reflecting on the contextual use of CAT within the EPS.